Abstract
Introduction: Sickle cell disease is a complex disease process highlighted by a high phenotypic variability associated with a myriad of acute and chronic complications. Cerebrovascular disease is a serious complication in SCD associated with a high degree of morbidity and mortality. The utility of transcranial doppler ultrasound (TCD) to measure velocity within major arteries of the brain has been validated as a way to predict those at increased risk for stroke. Unfortunately, despite the availability of TCD, individuals may develop stroke and/or silent stroke prior to obtaining an abnormal study. Hemolysis via a hemolytic index variable has been shown to be associated with other complications associated with SCD. This study aimed to evaluate an association between a hemolytic index variable obtained in the first two years of life and development of abnormal or conditional TCD velocities later in childhood in patients with sickle cell anemia (SCA) with thoughts this may provide an earlier tool to determine those who may be at increased risk for stroke prior to either obtaining a TCD or developing an abnormal TCD.
Methods: This study was a single-center, retrospective chart review of patients with SCA receiving their disease related care at our center over a 17 year period. Laboratory values, including lactate dehydrogenase (LDH), aspartate aminotransferase (AST), total bilirubin (TB), absolute reticulocyte count (ARC), and hemoglobin (HB), obtained in the first two years of life were extracted; these values were utilized to calculate a hemolytic index (HI) via principle component analysis to determine if a relationship existed between HI and development of conditional or abnormal TCD. All TCD results obtained from 2-14 years of age were also extracted from the patient's record. Cox proportional hazards models were then used to determine if the hemolytic index was a risk factor for abnormal or conditional TCD results.
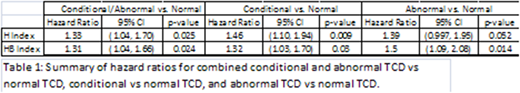
Results: A total of 193 patients with SCA between ages 2 - 21 years were reviewed with 109 included in the analysis. Laboratory values were averaged from included patients, then principle component analysis was used to find a linear combination of LDH, AST, TB and ARC to calculate a HI. The HI accounted for 49% of the total variation and had a correlation of 0.58 with mean LDH, 0.38 with mean AST, 0.46 with mean TB and 0.56 with mean ARC. Cox regression hazards model utilizing HI revealed a hazard ratio of 1.33 (95% CI 1.04‐1.70, p = 0.025) for developing a conditional or abnormal TCD velocity.
HB was then included along with the other four laboratory values for principle component analysis in creation of a hemoglobin HI (HHI); in this case, the index accounts for 44% of the total variance and it has a correlation of 0.52 with mean LDH, 0.33 with mean AST, 0.38 with mean TB, 0.55 with mean ARC and ‐0.42 with mean HB. Cox regression hazards model utilizing HHI revealed a hazard ratio of 1.31 (95% CI 1.04‐1.66, p = 0.024).
Conclusions: This retrospective study noted an increased risk for development of an abnormal or conditional TCD with an increased HI. The addition of hemoglobin to the HI to form HHI showed an elevated risk for abnormal or conditional TCD to the same degree as HI itself. These results could offer an additional tool in the evaluation of the pediatric SCA population, although these results would benefit from a prospective look. Further look into a possible association between HI and other SCD related complications such as stroke and acute chest syndrome could provide further information for the treating team for the overall management of this complex disease.
Woods:Global Blood Therapeutics: Research Funding; Pfizer: Research Funding; Guidepoint: Honoraria; Putman: Honoraria; Children's Mercy Hospital: Employment, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.